Past Issues
Fatal Case of Gestational Trophoblastic Tumour Following a Molar Pregnancy in a Low Resource Setting: A Case Report
Olivier Mulisya1,*, Kasereka Tatumwa Liston2, Katembo Mathina Erickson2, Kambale Kalungero Gervais2,3, Kavira Zawadi Iza2,4, Mwiraghulu Mumbere ghislain2, Mathe Jeff K5
1Department of Gynecology and Obstetrics, Fepsi hospital, Butembo, Democratic Republic of the Congo
2Department of Gynecology and Obstetrics, Centre Hospitalier Ngothe, Democratic Republic of the Congo
3Department of Gynecology and Obstetrics, Université Oficielle de Ruwenzori, Democratic Republic of the Congo
4Institut de bâtiments et travaux publiques de Butembo, IBTP, Democratic Republic of the Congo
5Université des Pays des Grands Lacs (ULPGL), OBS/GYN Department, Democratic Republic of the Congo
*Corresponding Author: Olivier Mulisya, Department of Gynecology and Obstetrics, FEPSI hospital Butembo, Democratic Republic of the Congo; Email: [email protected]
Received Date: September 16, 2023
Publication Date: October 17, 2023
Citation: Mulisya O, et al. (2023). Fatal Case of Gestational Trophoblastic Tumour Following a Molar Pregnancy in a Low Resource Setting: A Case Report. Oncogen. 6(2):26.
Copyrights: Mulisya O, et al. © (2023).
ABSTRACT
Hydatidiform mole is the most common gestational trophoblastic disease. The major risk of this disease is the constitution of a malignant gestational trophoblastic tumor with a poor prognosis if it is not detected and treated in time.
The main challenges observed were as follow: poor management of abortion, no means of biopsy, insufficient equipment, and the patient's poor adherence to care as well as her unfavorable socio-economic status.
These observations join those of other cases of molar pregnancy managed in similar conditions but with no reported adverse outcome.
Therefore, we encourage the implementation of strategies for regular training of health personnel, improvement of the technical setup, and community awareness for antenatal care from the first trimester of pregnancy to improve early diagnosis and proper management of hydatidiform mole in the context of limited resources.
Its management in low- and middle-income countries faces too many challenges that do not allow adequate management increasing the risk of complications such as persistent trophoblastic disease or malignant tumors.
We report the difficulties encountered in the management of molar pregnancy in rural areas in the eastern part of the Democratic Republic of Congo (DRC).
Keywords: gestational trophoblastic tumor, molar pregnancy, low resource setting, case report
INTRODUCTION
Gestational Trophoblastic Disease (GTD) is defined as a heterogeneous group of interrelated lesions arising from the trophoblastic epithelium of the placenta after abnormal fertilization.
It includes various lesions such as pre-malignant lesions including hydatidiform mole (partial and complete type), while malignant lesions (gestational trophoblastic neoplasm) comprise invasive mole, choriocarcinoma, Placental site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor [1]
The incidence is higher in women younger than 20 years and older than 40 years of age. It is also higher in nulliparous women, in patients of low economic status, and in women whose diets are deficient in protein, folic acid, and carotene [2].
The malignant lesions are often referred to as Gestational Trophoblastic Tumors/Neoplasms (GTN) [3]; Their prognosis is generally good but relies on accurate diagnosis, adequate treatment, and thorough posttreatment surveillance for early diagnosis of complications [4].
GTD management requires a competent healthcare structure, with a clear diagnosis, treatment, and surveillance guidelines, to ensure optimal care for patients [4].
Table 1: The FIGO prognostic system for gestational trophoblast tumours.
|
FIGO scoring |
0 |
1 |
2 |
4 |
|
Age (years) |
<40 |
>40 |
- |
- |
|
Antecedent pregnancy |
Mole |
Abortion |
Term |
- |
|
Interval months from end of index pregnancy to treatment |
<4 |
4<7 |
7<13 |
13 |
|
Pretreatment serum hCG (IUI-) |
<103 |
103<10 |
104<105 |
> 105 |
|
Largest tumour size, including uterus (cm) |
<3 |
3<5 |
>5 |
|
|
Size of metastasis |
Lung |
Spleen, kidney |
Gastro-intestinal |
Liver, brain |
|
Number of metastases |
- |
1-4 |
5-8 |
>8 |
|
Previous failed chemotherapy |
- |
- |
Single drug |
Two or more drugs |
CASE REPORT
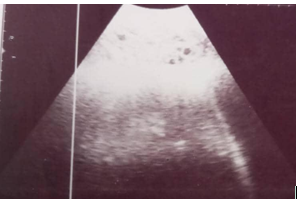
We report a 19-year-old woman admitted with vaginal bleeding and low abdominal pain with a history of amenorrhea. The serum beta hCG was 447mUI/ ml. The Ultrasound Scan demonstrating multiple intrauterine echoes with no fetus (snowstorm pattern).
Figure 1: Ultrasound scan showing the uterus content.
In her history, she was managed six months ago in the same context by a laparotomy with hysterotomy which was done to evacuate the intrauterine vesicular mass.
Two months later, her general condition was not improved, and the uterine mass reappeared with vaginal bleeding, the patient was put on vincristine without improvement, and she was then referred to our hospital for further management.
This patient fell into the low-risk prognostic group according to the FIGO prognostic scoring system for gestational trophoblast tumors with a score of 4 (Interval months from end of index of pregnancy to treatment : 1, largest tumour size inclunding uterus : 1 and previous failed chemotherapy : 2 )
The Manual vacuum aspiration guided by an ultrasound scan with accompanying syntocinon infusion was attempted from our setting but in vain, a sample was taken to Uganda for biopsy, but the results came out inconclusive.
Meanwhile, the patient was put on methotrexate 50mg 3 times per week, and folinic acid 3 times per week. The patient started reporting general body weakness and was having vaginal bleeding on and off. She received 4 units of blood as the hysterectomy was already indicated but she continued to bleed profusely to death.
DISCUSSION
Gestational Trophoblastic Disease (GTD) management requires clear guidelines for diagnosis, treatment, and follow-up [5].
The diagnosis, treatment and follow-up for our case did not meet the international standards due to poor knowledge and lack of resources.
Gestational trophoblast disease covers a distinct group of unusual but connected placental trophoblastic disorders with a variety of histological and clinical departments.
Regular follow-up patients have healed entirely while problems, delaying recovery, and not being properly treated relate to mortality [4].
Most women with molar pregnancy can be cured by removal of the products of conception and fertility is preserved [6].
Suction curettage is the preferred method of evacuation. Strict compliance with post-molar pregnancy surveillance is essential because of the potential development of gestational trophoblastic tumors (GTT) [7].
In our context there is no emphasis on different clinical protocols for the management of GTD, many cases of abortions are done without taking a biopsy. All hospitals around do not have pathologists, in all the province of North Kivu, we could have one in Goma town, 360km from Butembo.
Oncologists are nowhere in the region and chemo drugs are not affordable.
Unequal management skills among practitioners, inadequate treatment, irregular surveillance, and drop-out are common in resource-limited settings and can lead to life-threatening complications and morbidities [5].
We are now encouraging clinicians to use Manual Vaccum Aspiration for the management of abortions but not all hospitals can have the sets. This could be for help as a biopsy is taken instead of going for hysterotomy.
CONCLUSION
The management of GTD is too challenging in low-resource countries, from hospital settings to communities with poor involvement in follow-up. It is therefore imperative that healthcare resources, policies, and planning focus be coordinated rationally. Advocacy and the political will to invest in the development of human resources and healthcare infrastructure appear critical to gynecological cancer control and reducing the burden of disease in our region. A collaboration of clinicians with Ministry of health may organize a plan to train practitioners to harmonize practices.
A strong coalition between governments, experts, communities, and donor agencies will be needed to achieve these goals
Establishing a reference center for gestational trophoblastic diseases (GTD) in Eastern DRC could be an achievement.
ACKNOWLEDGMENTS
We acknowledge the whole team involved in the care of this patient.
AUTHORS’ CONTRIBUTIONS
The concept of this case report was developed by the corresponding author. Dr Kasereka Tatumwa Liston, Dr Katembo Mathina Erickson, Dr Kambale Kalungero Gervais, Dr Kavira Zawadi Iza, Dr Mwiraghulu Mumbere Ghislain were involved in the management and follow-up of the patient. Dr Mathe Jeff contributed in editing of the manuscript and was the team supervisor. In the preparation of the document, all authors were involved in the literature review and in critically reviewing the article.
FUNDING
None to disclose.
AVAILABILITY OF DATA AND MATERIALS
Anonymized data are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
Approved by the Centre Hospitalier Ngothe Ethics and Research Committee.
CONSENT FOR PUBLICATION
A written informed consent was obtained from the patient for the publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
COMPETING INTERESTS
The authors declare that they have no competing interests.
REFERENCES
- Jagtap SV, Aher V, Gadhiya S, Jagtap SS. (2017). Gestational Trophoblastic Disease - Clinicopathological Study at Tertiary Care Hospital. J Clin Diagn Res. 11(8):EC27-EC30.
- Mulisya O, Roberts DJ, Sengupta ES, Agaba E, Laffita D, Tobias T, et al. (2018). Prevalence and Factors Associated with Hydatidiform Mole among Patients Undergoing Uterine Evacuation at Mbarara Regional Referral Hospital. Obstet Gynecol Int. 2018:9561413.
- Akakpo PK, Ulzen-Appiah K, Agbeno E, Derkyi-Kwarteng L. (2017). Diagnosing and treating rare lesions in a low resource setting: lessons from a hybrid epithelioid trophoblastic tumor and choriocarcinoma. Ghana Med J. 51(4):196-199.
- Khachani I, Alami MH, Bezad R. (2017). Implementation and Monitoring of a Gestational Trophoblastic Disease Management Program in a Tertiary Hospital in Morocco: Opportunities and Challenges. Obstet Gynecol Int. 2017:5093472.
- Fatima S, Shaikh AG, Mahar T, Bozdar HUR., Memon S, Khokhar M. (2021). A Study of Molar Pregnancy at Low Resource Settings of Tertiary Care Hospital Sindh. Hypertension. 6:13-14.
- Gueye M, Ndiaye-Gueye MD, Kane Gueye SM, Moreau JC. (2016). Fatal cases of gestational trophoblastic neoplasia in a national trophoblastic disease reference center in Dakar Senegal. Int J MCH AIDS. 5(1):32.
- Riadh BT, Abdellatif C, Wissal H, Leila A, Taher M, Abdelhamid K. (2009). Clinical analysis and management of gestational trophoblastic diseases: a 90 cases study. Int J Biomed Sci. 5(4):321.
 Abstract
Abstract  PDF
PDF